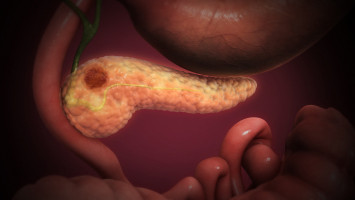
Many pancreatic tumours are like malignant fortresses, surrounded by a dense matrix of collagen and other tissue that shields them from immune cells and immunotherapies that have been effective in treating other cancers.
Employing bacteria to infiltrate that cancerous fortification and deliver these drugs could aid treatment for pancreatic cancer, according to newly published findings from a team of University of Wisconsin–Madison researchers.
Here's what to know:
Tumour collagen is a tough barrier: Pancreatic cancer is well known for its deadliness and has among the lowest five-year survival rates among common cancers.
While there are several drivers behind the disease's dismal prognosis, one that's the focus of this study is the matrix surrounding many pancreatic tumours, which acts as an effective barrier against treatment.
A bacteria-based infiltration: Hu is an expert in engineering cells for use as potential therapeutics or delivery vehicles for drugs.
For this study, published in April in the journal Med, Hu's lab applied a bacterium that could both penetrate through the tough collagen barrier and deliver immunotherapeutic "nano-drugs."
Approach shows promise in animal models: The UW–Madison team tested its E. coli-based delivery system in mouse models of pancreatic ductal adenocarcinoma, or PDAC, the most common and lethal form of pancreatic cancer, which was the focus of the study.
While this therapeutic approach shows promise for treating pancreatic cancer and other malignancies with tough collagen barriers, Hu's team is working on improving and simplifying it in animal models, with potential clinical trials still some time out.
Source: University of Wisconsin-Madison
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.