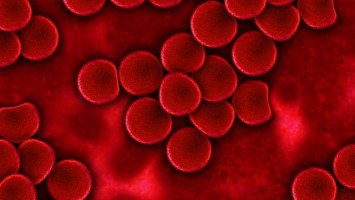
A novel combination of two cancer drugs has shown great potential as a future treatment for patients with acute myeloid leukaemia (AML), one of the most common types of blood cancers.
A new study by WEHI researchers has revealed the combination of two existing drugs eradicated AML cancer cells in lab-based tests.
The discovery, published in Cancer Cell, could soon lead to clinical trials, providing hope for the 1100 Australians diagnosed with AML annually.
WEHI researchers have for the first time tested a dual drug combination against AML, which proved highly effective in killing cancer cells in lab-based tests.
The researchers treated cancer cells with a combination of venetoclax, a current standard-of-care drug for AML, and a STING agonist, an emerging class of immunotherapy drugs.
This drug combination was notably successful against the more aggressive and difficult to treat forms of AML. This discovery may also change the way STING agonist drugs are used to treat other cancers.
Stimulating the ‘cell death enforcer’
The WEHI research team paired venetoclax, a current standard-of-care anti-cancer drug for AML, with a STING agonist, an emerging class of immunotherapy drugs. Venetoclax was based on a landmark research discovery at WEHI.
Study co-first author Dr Sarah Diepstraten said the team examined a range of different blood cancers, including cancer samples from patients with AML and treated them in the lab with the drug combination, leading to striking results.
“It’s really impressive - combining venetoclax with this emerging immunotherapy treatment can actually eradicate AML,” said Dr Diepstraten.
“This is the one-two punch combo that could be the knockout blow for AML. You could almost paraphrase the famous boxer Muhammed Ali and say this treatment floats like a butterfly, and STINGs like a bee.”
Critically, the combination treatment showed high promise in AML samples that were driven by a mutated p53 protein, a type of AML that is generally more aggressive and harder to treat.
The p53 protein plays a critical role in our bodies. When it is working effectively, it prevents the formation of cancerous cells by enforcing the death, or arresting the growth, of cells that have become damaged or abnormal.
But when the p53 protein is mutated and becomes defective in groups of cells, it can significantly boost a person’s risk of developing cancer.
Mutations of p53 are thought to be the biggest driver of cancer development and are found in half of all human cancers around the globe.
As cancers associated with p53 mutations tend to be more aggressive and resistant to treatment, there is a critical need for better therapies.
“For AML patients that do not have as much therapy-induced death of their leukaemia cells due to this mutated protein, combining venetoclax with a STING agonist causes more killing of AML cells than treating with venetoclax alone,” said Dr Diepstraten.
“The treatment was highly effective at killing cancer cells in samples with and without the p53 mutation, which is exciting given the lack of effective treatments for aggressive cancers driven by mutations in p53.
“We want to see more and more patients getting into long-term remission from blood cancers like AML, and we think adding STING agonists to the treatment regimen could be the key.”
A STING in the cancer tale
Associate Professor Gemma Kelly, co-senior author on the study, said that both venetoclax and the STING agonists played complementary roles in killing cancer at the cellular level.
“Within a cancer cell, venetoclax blocks the machinery of the cell that is keeping it alive. In certain blood cancers where this response is sub-optimal, STING agonists can supercharge this effect to deliver cancer a deathly blow,” Assoc Prof Kelly, a laboratory head in WEHI’s Blood Cells and Blood Cancer division, said.
“It is these two drugs, working in tandem, that led to the highly effective killing of AML cancer cells in our lab-based tests, in results that were truly striking.”
WEHI lab head Professor Andrew Wei, co-senior author on the study, said that while further research was needed, the findings were highly promising.
“While early clinical trials in solid cancers have suggested STING agonists are well tolerated in the body, these results offer exciting new hope for patients with the most resistant forms of leukaemia,” said Prof Wei.
“Given STING agonists are currently in clinical trials, we hope to conduct human studies using STING agonists in combination with venetoclax in the near future.
“The research findings are important, as they will inspire a completely new clinical approach for patients affected by the most resistant and deadly forms of acute leukaemia.”
WEHI researchers and clinicians are now translating these highly promising findings into a new clinical trial in AML patients in collaboration with Melbourne-based Aculeus Therapeutics, a local biotechnology company with a proprietary STING agonist.
Dr Mark Devlin, CEO of Aculeus Therapeutics, which has spent the last several years developing a potent STING agonist, couldn’t be more excited about the potential for the recent WEHI discovery.
“Drug discovery and development is the ultimate scientific team sport,” he said.
“Aculeus has developed a promising new drug but the collaboration with the WEHI teams, that have a deep understanding of the disease biology and the clinical landscape, will help shape how that drug will be used most effectively.”
Aculeus’ STING agonist, ACU-0943, is expected to enter clinical development for the treatment of AML later this year.
Source: Walter and Eliza Hall Institute
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.